Stanford University – Lead Investigator Dr. Justin Annes
Annes Lab Research Abstract
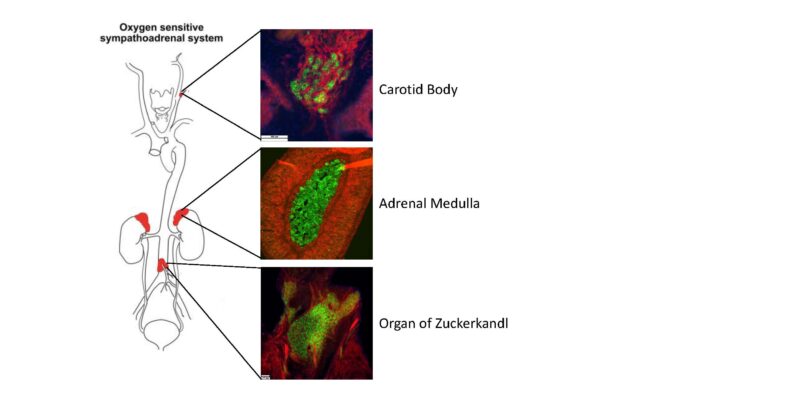
Inherited mutations in Succinate Dehydrogenase genes (SDHx) are responsible for a constellation of tumors including pheochromocytoma and paragangliomas (PPGL), renal cell carcinoma (RCC) and gastrointestinal tumors (GIST). Notably, tumors that result from an inherited pathogenic SDHB gene mutation have substantial metastatic risk, estimated to be ~40-50%. Unfortunately, effective treatments for metastatic SDHB-related disease are lacking. Indeed, a critical step along the therapeutic development pathway is establishing an animal model that faithfully recapitulates disease and facilitates therapeutic discovery. Although, numerous efforts over the past 20 years failed to generate an SDHB-deficient PPGL mouse model, leading many to conclude its impossibility, we recently succeeded in producing the first SDHB-deficient PPGL mouse model by co-deletion of SDHB and the NF1 tumor suppressor gene. We found that isolated SDHB deficiency was not sufficient for tumorigenesis, despite sharing many key features of SDHB-deficient tumors, such as mitochondrial swelling, histone hypermethylation and succinate accumulation. These findings led us to conclude that SDHB-deficient tumorigenesis requires disruption of additional, unidentified, tumor suppressor gene(s) that promote cellular replication and enable succinate-dependent cellular and metabolic reprograming (DNA hypermethylation).
The Annes Lab is pursuing three key areas of investigation advance SDHB research and the care of SDHx familes.
Project 1. Develop enhanced mouse models of SDHB-deficient pheochromocytoma /paraganglioma (PPGL). Specifically, the Annes lab is testing the role of novel candidate tumor suppressor genes (TSGs) in tumor formation. We have selected candidate TSGs based upon suspicious findings which suggest they play a critical but unrecognized causative role in SDHB-PPGL formation, e,g. they demonstrate reduced expression in human SDHB-deficient PPGLs. These candidate TSGs are being tested individually and concurrently with disrupted SDHB expression in mouse chromaffin cells. This research objective is of critical importance to the SDHB field because advancing new depends upon an accurate understanding of how SDHB-PPGLs form and grow, and having an animal disease model in which new therapeutic candidates can be tested. Currently, the lack of an SDHB-PPGL animal model is slowing progress towards a cure.
Project 2. Perform chemical and genetic screening to identify drugs and drug-targets that are uniquely cytotoxic towards SDHB-deficient cells. We hypothesize that SDHB deficiency creates fixed, cell-autonomous vulnerabilities that are amenable to selective targeting, i.e. opportunities to realize synthetic lethality. We are exploiting the complementary strengths of chemical and genetic screening approaches to discover pathways that maintain SDHB-deficient cell viability. This research objective is critical to opening new avenues of therapeutic development for SDHB-cancers.
Project 3. Develop an experimental assay for determining the function (pathogenicity) of SDHB variants of uncertain significance (VUS) and assesses potential genotype-phenotype relationships. Because roughly forty percent of known SDHB mutations are VUSs, numerous at-risk patients/families are left in a quandary after receiving their genetic test results. They do not know whether they are at risk for tumors or not. We are developing an SDHB functional assay that can be used to determine the pathogenicity of VUSs and improve care for currently unrecognized, but at-risk, SDHB families. Furthermore, our experimental system provides an experimental platform for uncovering potential genotype-phenotype relationships.
Collectively, the Annes Lab is addressing high priority fundamental, translational and clinical gaps in our understanding of SDHB-cancers with the intent of transforming the future outlook for affected individuals.